Why Attend?
Network
- Smaller, more intimate conference where you are much more likely to meet and spend time with professionals who can impact your career
- Special networking events designed to connect early-career professionals with mid- to late-career professionals
Learn
- Content is balanced between current clinical practices and the latest scientific research
- The widest range of sports-focused information
Featured Programs
Get a load of this!
Applying appropriate loads across the continuum of lower extremity rehabilitation
- Marisa Pontillo, PT, PhD, DPT, SCS
- Laura Opstedal, PT, DPT, OCS, SCS, USAW-2
- Daniel Larson, PT, DPT, ATC, SCS, CSCS
Collaboration Through Innovation:
Creating Novel Clinical Service Delivery Though Interprofessional Education, Research, and Community Partnerships
- Caroline Brunst, PT, DPT, AT
- John DeWitt, PT, DPT, AT
- Stephanie Di Stasi, PT, PhD
- Greg Hock, PT, DPT, OCS
Neuroplasticity across concussion management:
Enhancing assessment and functional task specific training utilizing the clinical trajectory model of recovery
- Rebecca Bliss, PT, DPT, DHSc
- Alex Habegger, PT, DPT
You Throw How Hard?
Treating the Baseball Athlete
- Marisa Pontillo, PT, PhD, DPT, SCS
- Mike Reinold, PT, DPT, ATC, CSCS
- Eric Bellm, PT, DPT, OCS
Click the icon for the full schedule! 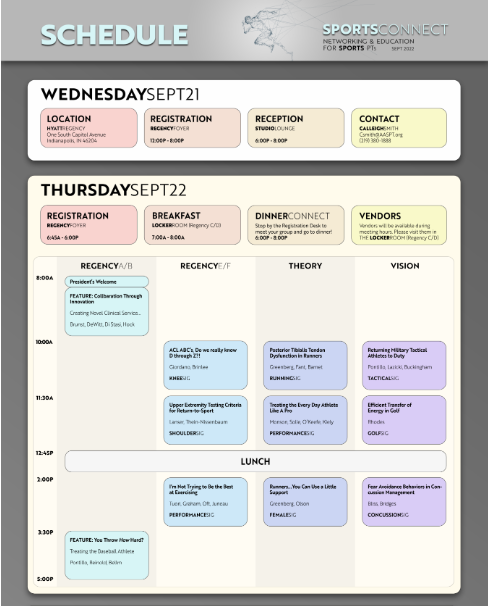
Pricing
|
Pre-July 15 |
July 16 |
Aug 16 |
| Student-Members: |
$200 |
$250 |
$300 |
| Members: |
$400 |
$450 |
$500 |
| Non-Members: |
$500 |
$550 |
$600 |
Registration includes access to any recorded programs from the conference that we post in our Learning Center after the event.
Hotel
Hyatt Regency Indianapolis
One South Capitol Avenue Indianapolis, IN 46204
The nightly room rate is $162.00++ To book your stay within the discounted AASPT room block, click the button below. The hotel room block cutoff date is Monday, August 15, 2022. Please note that the AASPT rate will not be honored after this date.
Book my Room
Click here to read the full terms and conditions. Please note the cancelation policy:
All cancellation requests must be in writing and sent to AASPT’s Director of Member Engagement. Cancellations received at or before August 22, 2022, 11:50 EDT (30 days prior to the start of the event) will receive a full refund. There is a $100.00 cancellation fee for cancellations received after August 22, 2022, and at or before September 11, 2022 11:59 EDT (10 days prior to the start of the event). No refunds will be made for cancellations received on or after September 11, 2022.
Important!
Many of these events have limited seating—particularly the DinnerConnects and the Break-Out Sessions. Make sure you grab your seat when you register!
|
